One issue that’s constantly pushed by the media about the effects of COVID-19 is that it’s much more deadly for older people than for younger people. The following graph, for example, shows the age distribution for COVID-19 deaths in Italy as of 11, April:
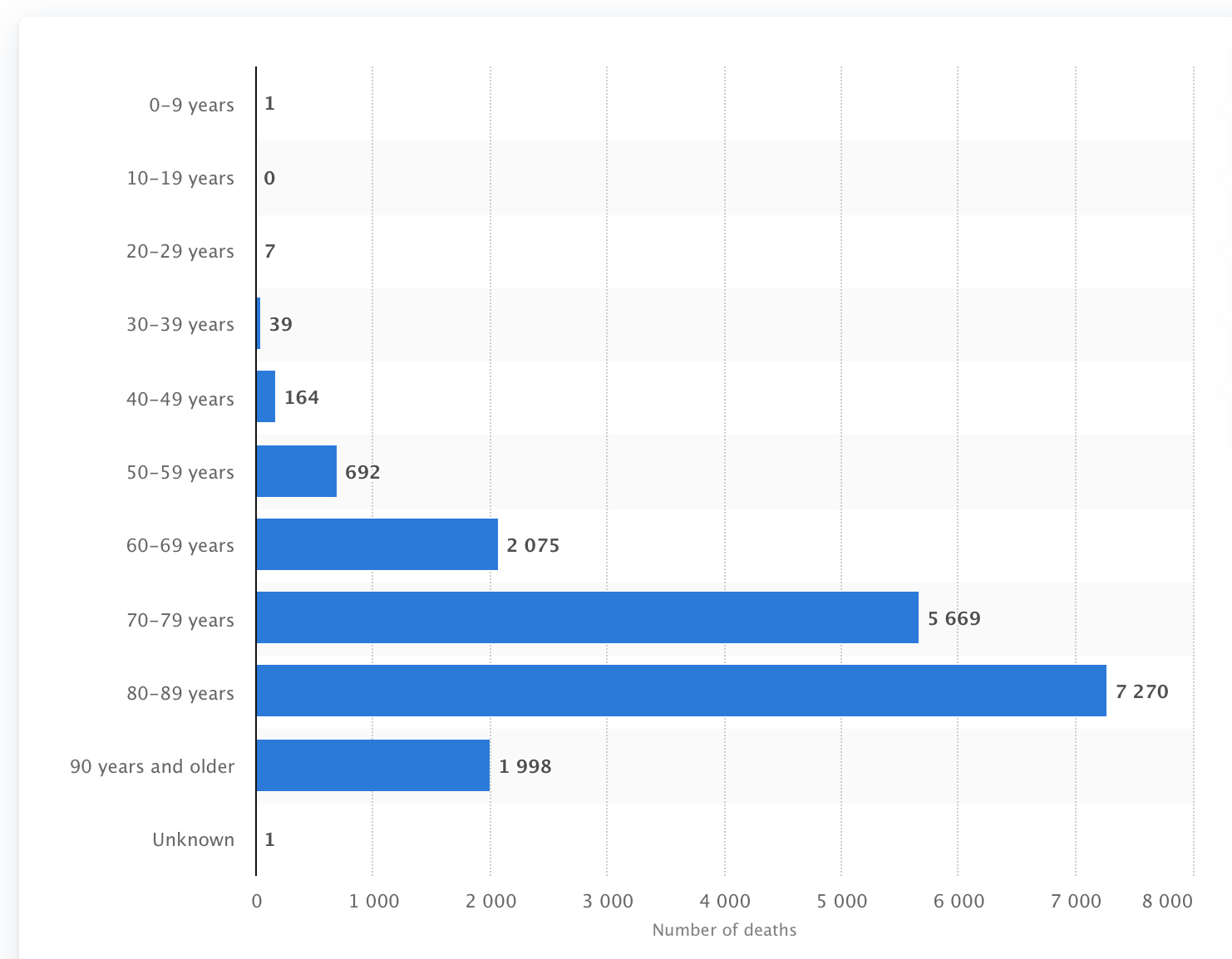
Bear in mind, also, that there are fewer people in the older cohorts, so the differences in the rate of deaths per cohort are even greater.
But does this suggest that COVID-19 is affecting younger and older people to a different extent? In one sense clearly yes – more older people are dying than younger people. But, in another sense, no. Or at least, possibly no.
In this article David Spiegelhalter – whose podcast I mentioned in an earlier post – considers the hypothesis that everyone’s risk of dying in the short term is affected by the current epidemic in exactly the same way, regardless of age.
Look, for example, at this diagram taken from David’s article:
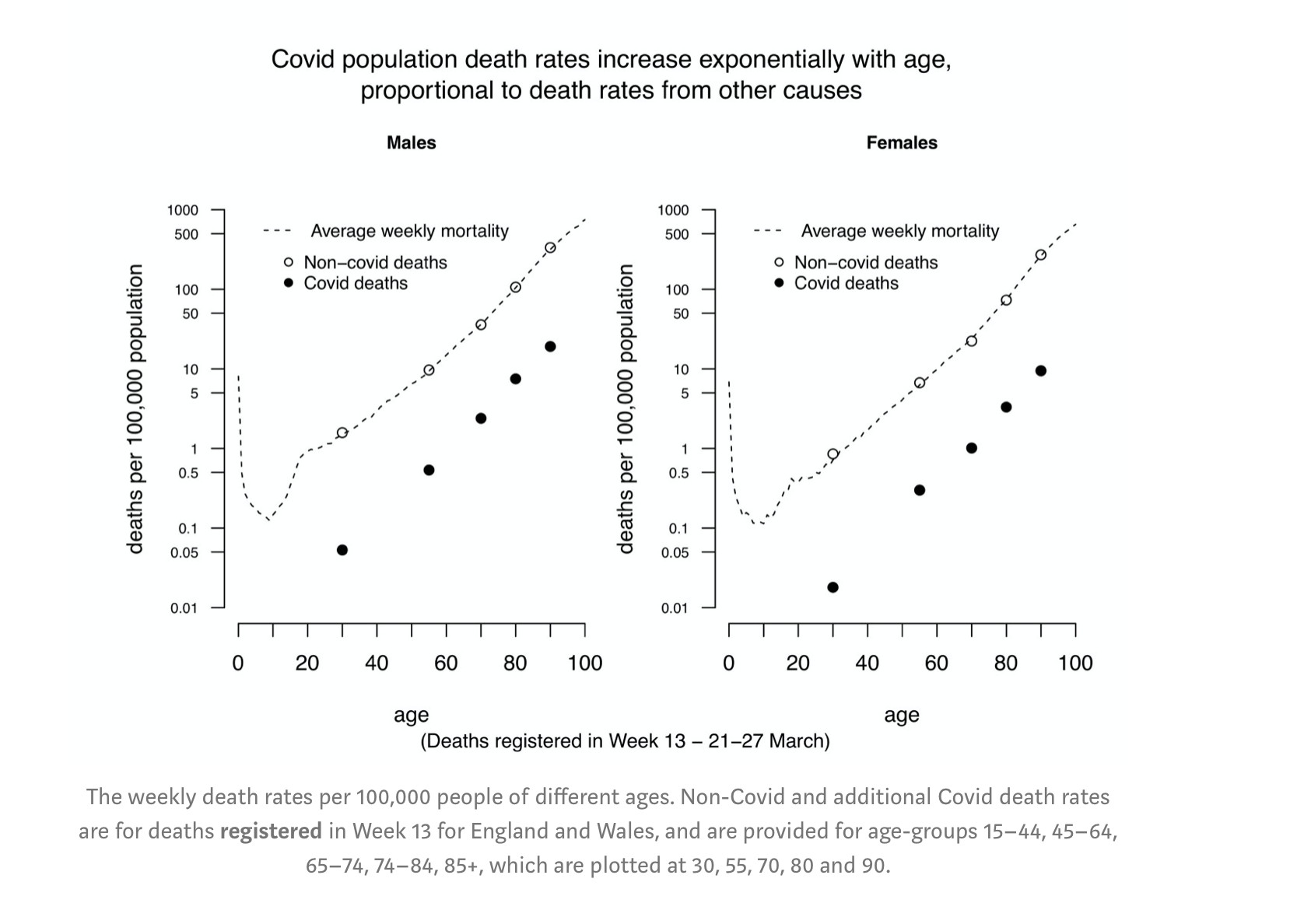
These are deaths by age, per 100,000 of the population in England for a week in March, shown separately for males (left) and females (right). The solid dots correspond to COVID-19 deaths, the hollow dots are all other deaths.There are several points to notice:
- The scale of the graph is logarithmic, so since the death counts – both COVID-19 and not – are approximately linear, the raw numbers will be increasing exponentially with age;
- This is true for both males and females;
- The patterns for COVID-19 deaths and others are roughly parallel on this logarithmic scale. This means that on a linear scale, one will be a multiple of the other.
Consider, for example, males in the 45-64 cohort. The death rates for COVID-19 and other causes are around .05 and 10 per 100,000 respectively. This means that the total risk of death including COVID-19 is 10.5:10 or 105% real-time to what it would have been with COVID-19 excluded. Loosely speaking, COVID-19 has raised the death risk for someone in that cohort by around 5%. But if you look at any of the other cohorts, the change is around the same. For example, in the 65-74 cohort, the respective death rates are around 2 and 40 per 100,000, leading to a ratio of 42:40 which is again 105%.
So, looked at this way, COVID-19 is affecting people of all ages in exactly the same way: it’s increasing the risk of death by around 5%. It’s simply that the death risk is so low for young people that an increase of 5% doesn’t lead to many additional deaths in absolute terms, whereas for older people a 5% increase in death rate leads to substantial increases in the observed numbers of deaths. Nonetheless, this provides an interpretation by which COVID-19 is non-discriminatory in terms of age.
A few caveats:
- This analysis is based on relatively few data. Though David’s article includes other analyses to support the hypothesis, he also concludes that further data will be required to verify it.
- Most of the deaths observed in the data summarised above will have been for people infected prior to lockdown measures having been introduced. It’s likely to be the case that lockdown measures will offer more protection to certain age cohorts than others, in which case the effect on death rates will be disproportionate across age cohorts.
- David also mentions in his article that health workers appear to be disproportionately affected in terms of COVID-19 – i.e. their additional death risk due to COVID-19 is greater than 5%.
